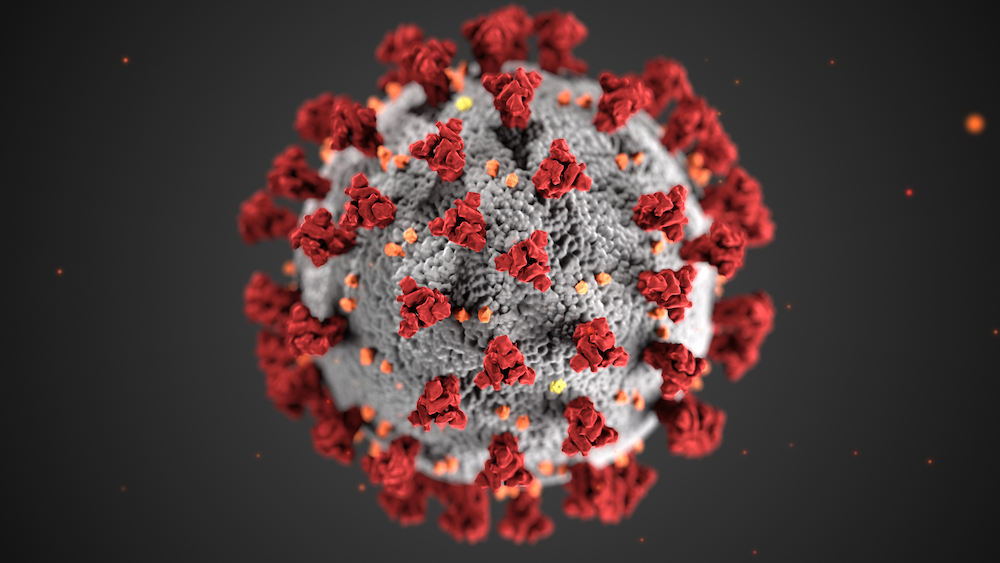
We are sleepwalking into a public health disaster. I’m living through a small part of it—not nearly as bad as many—and it’s enough to scare the daylights out of me.
I had Covid in January, as I was preparing to move from San Francisco to Hilo, Hawaii. Vaxxed and boosted, I felt like crap for about a week but was never in serious danger. Then my symptoms abated, my test turned negative, and it seemed like it was over. I’d had a classic “mild” case. Or so I thought.
In May I suddenly began having pain in my right knee, bad enough that it made it difficult to get up and down the stairs in my new home. Happily, I had a medical appointment already scheduled for just a couple days later, so the knee problem became item number one on the agenda.
My primary care provider, a very sharp advance practice R.N., ordered an X-ray, which showed nothing unusual. She gave me some strengthening exercises to do and thought it would likely get better over time—just one of those things that happens sometimes.
No such luck. A few days later it wasn’t just the one knee: Both knees and both ankles were now stiff and painful. As days went by it became clear that it wasn’t just the knees and ankles, but that all the little joints in my feet were affected, too. Everything from the knees down was stiff and sore all the time. Being on my feet a lot made it worse.
On the bright side, the pain was now not quite as severe as the initial knee pain, but it was constant, and bad enough to limit my mobility. I also began to experience fatigue and loss of stamina. I’d be okay in the morning, but sometime after lunch I’d just crash and need to lie down—something I’ve never experienced before.
Having made my living as a health reporter for some years, I immediately began wondering about Long Covid, since fatigue and joint pain are commonly reported Long COVID symptoms. And though I wasn’t experiencing the crushing fatigue that some long-haulers report, I had definitely been jarred out of my usual state of being, with no other obvious explanation.
My provider was skeptical at first—not unreasonably. The problem with long Covid is that the symptoms it produces can also be caused by lots of other things, and sorting them out can be difficult. There’s no simple diagnostic test; it’s a process of elimination. So, she ordered a set of blood tests looking for indicators related to arthritis, hoping for a clue.
The tests came back inconclusive. One marker, called Rheumatoid Factor, was elevated, but not as dramatically as is typical in rheumatoid arthritis. One other was a bit elevated, but most were in the normal range. It wasn’t a pattern associated with any “normal” arthritis-related condition. We’ll be repeating the tests in early September to see if there’s a trend that might give a clue.
For now, I’m in a sort of medical black box. Something is wrong enough to interfere with my life in significant ways: Walking fast is out of the question, as are things I used to love to do, like hiking or going for long walks in town. Whether I will ever be able to do those things again remains a mystery. What exactly is happening or what to do about it remains unclear
I’m far from alone. A CDC analysis of electronic health records that compared more than 353,000 Covid patients with a control group of non-Covid patients. The Covid survivors were far more likely to report a variety of conditions and symptoms in the period following their initial illness. For those aged 18-64, one in five “experienced at least one incident condition that might be attributable to previous COVID-19.” For those aged 65 and over the rate was one in four.
Conditions diagnosed in these Long Coviud patients ranged from kidney failure and potentially life-threatening heart and circulatory problems to diabetes, muscle and joint pain, and fatigue. These conditions, the CDC noted, could “affect a patient’s ability to contribute to the workforce and might have economic consequences for survivors and their dependents, particularly among adults aged 18–64 years. In addition, care requirements might place a strain on health services after acute illness in communities that experience heavy Covid case surges.”
Rates of Long Covid symptoms have varied between studies, with a few reporting even higher prevalence rates than the CDC found. A British Medical Journal preprint (meaning it hasn’t yet been peer-reviewed) reports on a survey of over half a million Covid patients, finding that 37.7 percent reported at least one symptom at least 12 weeks after the original illness and 14.8 percent reported three or more symptoms. Extrapolated to the entire British population, that would mean nearly 6 percent are experiencing Long Covid symptoms. The British researchers reported clusters of symptoms, with certain conditions, such as tiredness, difficulty sleeping, and muscle aches commonly occurring together.
A review of the medical literature underlines how little we know. Nature recently published a meta-analysis combining analyzing the results of multiple Long Covid studies and surveys, but researchers could only draw limited conclusions because the data thus far is incomplete, compiled using varying methodologies that make detailed analysis difficult. Perhaps most importantly, they note, “[T]he reason why some patients experience long-term symptoms after COVID-19 is uncertain.” Assorted theories have been suggested, but no one really knows what the hell is going on with patients like me.
For the U.S., the implications are staggering. We passed 90 million total Covid infections in July, with an average of more than 120,000 new infections reported per day. And that’s certainly a significant undercount as infections detected on home tests are usually not reported. But even using the most conservative numbers, 20 percent of 90 million means 18 million Americans with Long Covid symptoms, with about 2,400 being added to the total every day.
And this is happening while efforts to stem the tide of infection, like mask requirements in indoor spaces, have mostly been abandoned. The federal government could aggressively encourage masking and use the Defense Production Act to produce and distribute high-quality masks like N95s to every household, but it seems no one in authority wants to talk about preventing infection anymore. In a July 22 interview on Washington Post Live, CDC Director Rochelle Walensky couldn’t even bring herself to make a clear recommendation on wearing masks in crowded, indoor spaces.
Yale University epidemiologist Gregg Gonsalves laid out his frustration in a recent column for Time whose title sums it up: America Is All Too Happy to Let People Die. Asked about the impact of Long Covid given America’s trajectory, Gonsalves doesn’t hold back: “No one is taking Long Covid seriously. That would mean you have to take cases seriously… It’s a total disaster. We are walking into a mass disabling event because people are tired of the pandemic.”
Lisa McCorkell, co-founder of the Patient-Led Research Collaborative, shares Gonsalves’ frustration. The collaborative, formed by a group of Long Covid patients from very first wave of the pandemic who also had research backgrounds, published some of the earliest data on Long Covid patients and continues to pursue new research.
Seven-point-five percent of all adults in the US have Long Covid,” McCorkell says. “The fact that Long Covid is not being mentioned anytime Covid is mentioned, and is not being considered in Covid mitigation strategies and risk, is a disservice to the public and will result in millions more people developing Long Covid.”
So-called “mild Covid,” she adds, “is being normalized and accepted in order to ‘return to normal’ without any discussion on the large risk of getting Long Covid.”
This has consequences for everyone, but especially for the patients themselves, who may be seriously disabled but struggle to get disability benefits for an illness that is still poorly understood and lacks an agreed-upon definition. She notes parallels with early AIDS activists (who, of course, include Gonsalves), who also dealt with a medical community that had little to offer them and a government that preferred not to pay attention to the unfolding crisis.
What would she like to see done?
“To reduce the spread of Covid, I would employ data-driven mask mandates, improve the ventilation in public spaces, and include the risk of Long Covid in any policy decision related to Covid. To address Long Covid, I would ensure all workers have paid sick and family leave, reform disability benefits, encourage and enforce accommodations at work, start a public and clinical education campaign on Long Covid, increase funding for Long Covid clinical care (including to community health workers), and expedite and fund clinical treatment trials.”
Almost none of this is happening. Our leaders, apparently, have found it more convenient to keep sleepwalking toward disaster.