While I’m far from the only person worried about Long COVID and our society’s general inclination to look away and pretend it’s not there, people like me certainly feel badly outnumbered. It’s beginning to feel reminiscent of how people with AIDS and their loved ones felt circa 1986—and maybe it’s time for the same kind of response.
For those of you lucky enough not to have lived through that era, by the end of 1986, AIDS had killed nearly 25,000 Americans, but president Ronald Reagan had yet to speak the word “AIDS.” His press secretary had joked about it and the White House press corps laughed. While individual scientists were doing important work, the bureaucracies running the NIH and FDA seemed very much to be in business-as-usual mode. Because the casualties had largely been gay men and injection drug users, it seemed like no one with any power cared whether we lived or died.
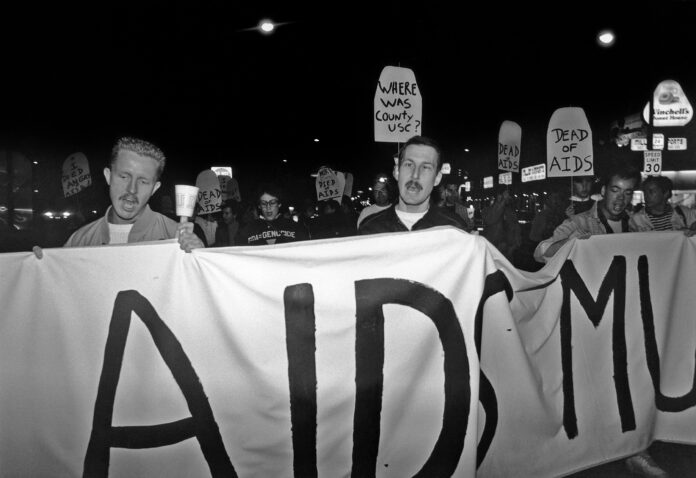
So, a group of New Yorkers – mostly gay men – decided it was time to start raising hell. Calling themselves ACT UP, they disrupted the New York Stock Exchange and, as chapters sprang up nationwide, they staged protests that shut down the FDA and NIH. Eventually, people like Anthony Fauci began to see they had a point. I joined the Los Angeles ACT UP chapter in 1988 and ended up getting arrested half a dozen times in protests at the LA federal building, the County Board of Supervisors and the U.S. Capitol, among others. We won major improvements in HIV/AIDS care in the Los Angeles County health system, which cared for thousands of people with AIDS who had no health insurance. When I landed in San Francisco in 1993, I connected with ACT UP Golden Gate.
Here I am (with my late boyfriend Tim at the left) at one of the protests in that L.A County healthcare campaign. Most of my closest friends from that era have been dead for decades.
I get that COVID has played out very differently than HIV/AIDS. AIDS ramped up slowly and seemed not to affect “normal” people until it killed closeted gay movie and TV star Rock Hudson in 1985, and even then officials largely looked the other way. Only scientific breakthroughs in the 1990s finally stemmed the tide of death. In contrast, the much more highly transmissible SARS-CoV-2 virus came on fast and furious, turning Americans’ lives upside-down almost immediately.
But now, we’ve arrived at what seems in some ways like an eerily similar place. When needed precautions to curb a highly infectious airborne virus spurred frustration and political pushback, officials largely threw up their hands and gave up. Even measures that don’t involve mandates or restrictions on behavior have mostly either been dropped or never happened in the first place.
LONG COVID’S GROWING TOLL
Unfortunately, the virus hasn’t gone away, even if the initial wave of mass death has receded. In August, as a summer surge peaked, US COVID-19 deaths exceeded 1,000 per week, though the latest September data suggests the numbers have begun declining toward pre-surge levels, when deaths were generally in the 300-400 per week range. That’s still equal to a 9/11 every eight to 10 days. Centers for Disease Control and Prevention tracking of SARS-CoV-2 levels in wastewater—probably the best data on US viral prevalence now that cases aren’t being reliably tracked—showed 15 states with “very high” levels and another 19 rated as “high” as of Sept. 19.
But COVID is not just a matter of cases and deaths. The disease’s long-term effects have disabled millions of Americans, and the numbers keep growing with each new wave of infection. An updated review published in Nature Medicine puts the current global number of Long COVID sufferers at 400 million and estimates the worldwide economic impact at a staggering $1 trillion.
We now have plenty of people experiencing repeated SARS-CoV-2 infections. The good news, if you can call it that, is that these reinfections may produce fewer new cases of Long Covid than a person’s first infection – but they absolutely produce some, and the Omicron variants circulating in the last year or two seem to produce more Long Covid than earlier viral varieties. Every time you get COVID, you roll the dice with your health – maybe for the rest of your life.
If I sound alarmed, well, I am. As longtime readers may know, I have some first-hand experience with Long COVID, though in milder form than many experience. My January 2022 infection left me with peripheral neuropathy—painful nerve damage—in my legs and feet. It’s incurable and nearly impossible to treat, as conventional pain drugs don’t help. I will likely never live another day without pain and walking more than six or seven blocks at a stretch is a struggle. I used to enjoy hiking, but will probably never do it again. Still, I don’t have the more debilitating symptoms like crushing fatigue or dysautonomia—disruption of the part of the nervous system that controls automatic functions like heartbeat, blood pressure, digestion and breathing—that afflict some Long COVID sufferers. Lots of people have it way worse than I do.
We know that COVID can have lasting impacts on many parts of the body, including the brain. A recent study of 52 COVID survivors—about half with mild to moderate initial illness and half with more severe disease—found that compared to healthy controls, both groups “had a significantly higher score of cognitive complaints involving cognitive failure and mental fatigue” 27 months after their original illness, with no significant difference based on the severity of that initial illness. On a series of tests, researchers found “changes in brain function” that may explain the reported problems.
Just as scary, a study of people aged 65 and up just published in the Journal of Alzheimer’s Disease reports that “people with COVID were at significantly increased risk for new diagnosis of Alzheimer’s disease within 360 days after the initial COVID diagnosis.” This review of the medical records of over six million patients found that the risk escalated with advancing age. As with many of these long-term impacts, the mechanisms involved remain unclear.
Survivors of an initial SARS-CoV-2 infection also have increased rates of high blood pressure, now documented in multiple studies. High blood pressure increases your risk of deadly cardiovascular complications like heart attack and stroke.
I can’t help but wonder whether these issues have affected me, but there’s no way to be sure. My blood pressure, well-controlled for a dozen years with a very low dose of medication, began ratcheting upward about a year and a half ago, necessitating three medication adjustments since then. I’m also definitely more forgetful than I was, mostly little things like walking into a room and forgetting why I went there. But those things can happen to older people with or without COVID, and it’s hard to know cause-and-effect in a given individual.
But I sure as hell know I don’t want to get this virus again and risk these and other issues getting worse. Unfortunately, avoiding it is getting harder by the day, and neither government at any level nor public health authorities seem to care.
PREVENTION? WHAT PREVENTION?
While there’s some evidence that the antiviral drug Paxlovid can reduce the likelihood of Long COVID if administered early enough, the results so far are mixed and not overwhelming. The best way to avoid Long COVID is to not get infected in the first place. As a society, we’ve pretty much stopped trying.
The government is still encouraging vaccination, as it should. But it’s been clear for some time that while the vaccines are very good at reducing the chance of severe illness and death if you get infected, they offer only limited protection against getting infected in the first place. “Vax and relax” can prevent mass death, but it can’t prevent mass infection and an ever-growing number of cases of Long COVID, even if most people get vaccinated. And vaccination rates have been declining for a while, with a new Ohio State University survey reporting that only 43% of U.S. adults have gotten or plan to get the new COVID-19 shot.
And in a bit of absolute madness, Florida’s Ron DeSantis-appointed Surgeon General Joseph Ladapo has actually advised against use of the newly updated mRNA vaccines. In a post on Mastodon, Yale epidemiologist Gregg Gonsalves called this “beyond irresponsible. It is malpractice.”
Ladapo is an outlier, but even his saner colleagues around the country downplay the fact that we don’t have to limit ourselves to vaccination. It’s an airborne virus, so there are two main ways to stop it from spreading: 1) Get the virus out of the air, or at least reduce its concentration to a very low level, and 2) Protect yourself from breathing in any virus that’s in the air around you. We know how to do both.
Masking works, but the type of mask matters. As the Mayo Clinic notes, “Respirators such as nonsurgical N95s give the most protection. KN95s and medical masks provide the next highest level of protection. Cloth masks provide less protection.” Two and a half years ago, a CDC study found that those who reported regularly wearing an N95 or KN95 respirator in indoor public settings had an 86% lower risk of catching COVID-19.
Recently, during my first return visit to San Francisco after moving in early 2022, I met my nieces for lunch at the Ferry Plaza. It was a Saturday, Farmers Market day, and the place was jammed. In three-plus hours I saw no more than half a dozen people wearing any sort of mask, and only a couple were N95s. In my new hometown of Hilo, masking is only slightly more common. At the supermarket, I see barely 10% of customers and staff in some sort of mask. In some venues, it’s less.
A recent Ipsos survey found that half of Americans believe they’ll never get COVID again. Only 20% described themselves as “trying to stay as safe as possible.”
None of this is a surprise—people are simply responding to the messages they get from the people supposedly leading on health issues. The CDC promotes vaccination but barely talks about masking anymore; it acknowledges the value of indoor air quality but doesn’t seem to be doing much about it. In interviews, CDC Director Mandy Cohen regularly urges vaccination but almost never brings up masking or air quality and says little about Long Covid. Political leaders mostly talk about COVID in the past tense and pat themselves on the back for a job well done in prior years. The result is what you’d expect: Most Americans now treat COVID like a common cold, disregarding most precautions and not bothering to test when they get sick.
Back in 2022, when public policy on COVID was still relatively sane, the Biden administration published indoor air quality guidance and made congressionally-approved funds available that “that can be used in schools, public buildings, and other settings to improve indoor air quality.” It’s unclear exactly how much of that money has been used and for what, although some school systems have definitely made HVAC upgrades. But we’ve never had either enforceable indoor air standards or a coordinated plan to implement them. As Science noted in July, “The COVID-19 pandemic has clearly shown the vulnerability of society to the spread of infectious diseases. At the same time, with frequent outbreaks in elder care facilities and school classrooms, it became clear that it was a fatal mistake to largely neglect the recommendations of scientists and engineers regarding minimum standards for ventilation and indoor air quality.”
In any case, those federal dollars were aimed at schools and public buildings. It’s been left entirely to the private sector to do, or not do, anything to reduce airborne pathogens in supermarkets, theaters, clubs, malls and other privately owned spaces. Local groups like Chicago’s Clean Air Club and Austin’s Clear the Air ATX have tried to fill the gap by lending HEPA filters and other clean air equipment to arts and performance venues and other gathering places.
A RADICAL IDEA: DO WHAT WORKS
We know what to do. As Clean Air Club founder Emily Dupree and co-author Shelby Speier wrote in Sick Times in May, “We possess the technology to make public spaces safer. Studies show HEPA air purification and far-UVC lamps drastically reduce the number of airborne pathogens in a room and therefore lessen the likelihood of COVID-19 transmission. When combined with other layers of protection, these tools have the potential to finally make our shared spaces more accessible during an airborne pandemic.”
A key word here is accessible. Failure to address indoor air quality and other prevention measures makes public spaces seriously dangerous for those at highest risk, including the elderly, the immunocompromised and those with long-term health issues, including Long Covid.
Such simple, factual messages are rarely heard in official statements about COVID. “What I find the most frustrating about official handling of COVID and prevention is the lack of care, education, and honoring the science around COVID,” comments Clear the Air ATX founder and Long Covid activist Katie Drackert. “Telling people to ‘stay home when they feel sick’ for a virus that spreads asymptomatically? Well, they are just straight up ignoring science.”
Admirable as they are, the small, volunteer-driven efforts of groups like Drackert’s and Dupree’s are not remotely comparable to the scale of the problem. For now, people must take matters into their own hands. “In the year 2024, people still need to be wearing a well fitted KN95 or above for optimal communal and individual protection,” Drackert says. In the absence of reliable information about air quality in indoor spaces, she suggests getting a portable air quality monitor, which can be reasonably affordable. “High CO₂ levels indicate poor ventilation, which may lead to higher concentrations of aerosols that could contain the virus,” she explains. “Some air quality monitors track particulate matter (PM2.5 and PM10), which are small airborne particles. While COVID is smaller than these particles, high PM levels may indicate poor indoor air quality.”
Most of us can’t entirely avoid being in spaces with poor air quality, and that leaves us with masking, which the country has largely abandoned. Worse, we’re starting to see bans on face coverings in public spaces being enacted—for example, in Nassau County, New York, and North Carolina.
These laws typically contain exceptions for people masking for health reasons, but, as New Jersey’s Star-Ledger noted in a recent editorial opposing a proposed mask ban, “[I]t leaves it up to the cops to decide whether someone has a legitimate medical reason for wearing a mask at a public gathering.
“How will they know that? It’s subjective. And based on past experience, we know what that means: Police will disproportionately stop and question Black and brown people, who have also been the most likely to continue wearing masks to protect against COVID-19.”
It’s hard to imagine a more demented public policy than making disease prevention illegal. And it’s not hard at all to imagine a COVID-19 prevention framework that would make a meaningful difference without causing a nationwide freakout:
Encourage masking. Even if mask mandates are a political non-starter, there’s still plenty we can do. First, officials can talk about it and actively encourage people to wear high-quality protection like N-95s when in busy, indoor spaces. They can remind people of its importance—that COVID is not over, not just a cold, and that even a “mild” case can change your life forever. Federal, state and local governments could distribute N-95s or KN-95s free or at minimal cost.
Get serious about indoor air purification. Build on what the Biden administration started a few years ago: Develop medically informed, enforceable indoor air quality standards and create a verification system so that people know when a building they enter meets them. Start with public buildings and the largest, busiest private venues, like sports arenas, concert halls and theaters, and move on from there. Give business owners generous technical and financial support in meeting those standards, and a reasonable amount of time in which to do it. While this program is ramping up, fund the local organizations now struggling with limited resources to fill the gap.
None of this is that difficult. It’s not even that expensive when you consider that the federal government is in the process of spending $634 billion to upgrade nuclear weapons that with any luck will never be used. What’s missing is political will, and that won’t be there until people scream bloody murder.
That’s why I think it may be time for a new version of ACT UP focused on COVID-19. The issues are somewhat different, but less so than you might think. While the original ACT UP focused a lot on research, treatment and care, it also addressed prevention. ACT UP chapters around the country started syringe exchange programs, handed out condoms at high schools, and sometimes succeeded in shaming the system into doing the right thing. And of course, there are issues to tackle around Long Covid research that I haven’t addressed here, but which I will try to cover in a future piece.
The fundamental problem is much the same as people with AIDS faced in 1986: a system stuck in neutral, politicians stuck in denial, and a public closing their eyes, covering their ears and shouting, “I don’t hear you!”
The first task must be to break the system–and the broader population, as much as possible–out of its present inertia, complacency and denial. I honestly don’t know whether ACT UP tactics like occupying the CDC and disrupting state and local health commission meetings will have the same effect they did decades ago, but at this point I don’t know what else to try. Nothing good lies at the end of our current path.